Insulin Resistance is related to obesity. Obesity is on the rise in the United States. BMI stands for “Body Mass Index”; BMI equals a person’s weight in kilograms divided by height in meters squared. (BMI=kg/m2). A person who has a BMI over 25 is considered overweight and a person with a BMI over 30 is considered to be obese.
Between 1976 and 2002 there has been a 38% increase in the number of American adults who are overweight and the number of obese Americans has doubled. About half of all Americans are overweight and 25% of Americans under the age of 40 are obese.
What is happening to children is even more disturbing. Between 1963 and 1970, 4% of children between 6 and 11; and 5% of children between 12 and 19 were overweight. In the period between 1999 and 2002 the number of overweight children in both groups was 16%–it had more than tripled. The figures are even worse, according to research according to a Yale University study published in New England Journal of Medicine March 14, 2002
- 20% of American children are overweight.
- 25% of children 4-10 years old and 21% of those 11-18 years old have early signs of Type 2 diabetes demonstrated through impaired glucose tolerance.
- Younger children are worse off than older.
A few words about insulin
Insulin is involved in fuel storage—it is an anabolic hormone. Glucose transports sugar into the cells. 80% of the body’s cells become permeable to glucose when insulin binds to receptors on the cell membranes. Sugar is phosphorylated and used as fuel. It is stored in the short term for later use of energy as glycogen. Excess sugar is converted to triglycerides and then to fat. In the presence of large amounts of insulin, we don’t burn fat, we deposit fat.
As stated, insulin is anabolic hormone. It promotes the uptake of amino acids and the subsequent formation of proteins. Insulin increases the rate of protein synthesis and decreases the rate of protein degradation. Thus, insulin deficiency will lead to increased catabolism of protein. Increased proteolysis leads to elevated concentrations in plasma amino acids that serve as precursors for gluconeogenesis.
Insulin has a half-life of 30-45 mins. and is fully cleared in about 6 hours. Effects may continue for hours and even days at the cellular level. Insulinase breaks down insulin in liver and kidney and is a zinc dependent enzyme. Breakdown of fat is greatly enhanced by the absence of insulin.
60% of glucose from food is stored in the liver. Once the liver is full, glucose is turned to fatty acids and packed as triglycerides in VLDL for deposition as fat.
Sugar consumption and insulin resistance go beyond the obvious problems of obesity, diabetes and high cholesterol. Sugar is also linked to fatigue, high blood pressure, fatty liver, atherosclerosis, yeast overgrowth, magnesium loss, acidic pH, calcium/phosphorus imbalance, polycystic ovary disease, endocrine problems, a systemic inflammatory state, impaired fibrinolysis and pro coagulation, and an environment that favors neoplastic (cancer) growth.
The average American consumes nearly 200 pounds of refined sugar each year, and we get half of our calories from refined carbohydrates. This creates vitamin deficiency and insulin insensitivity. Other factors that contribute to the metabolic syndrome include stress, poor sleep habits, lack of exercise, and exposure to toxins. Eating too much sugar causes the body to produce too much insulin. Over time, the body becomes insensitive to the insulin. Many of your health problems are due to excess insulin and to insulin insensitivity. Insulin insensitivity is responsible for obesity—and all of its associated health problems. Type 2 diabetes is due to insulin insensitivity. Unlike type 1 diabetes, which is a state where the body cannot produce insulin, type 2 diabetics produce insulin, but the body simply does not respond.
Insulin insensitivity can lead to serious health problems. It encompasses three conditions: metabolic syndrome (sometimes called syndrome X), adult onset (type2) diabetes and people who are insulin insensitive, but have not developed these conditions yet. Insulin has a lot to do with weight gain and so many other common health problems you see in your office. Sugar and insulin are involved with high blood pressure, high cholesterol, high triglycerides, type 2 diabetes, menstrual problems, heart disease, pain, inflammation, depression and even polycystic ovaries. With simple lifestyle changes and some good nutritional products you can help people to easily lose weight and help them with a lot of other health problems. This is easy and it works. Fortunately, it responds very well to nutritional therapy.
Symptoms of insulin resistance include fatigue, weight gain, brain fog, carbohydrate craving, and periods of hypoglycemia after a high carbohydrate meal (often needing a nap after eating). Approximately 50% of your hypertensive patients are insulin insensitive. Approximately 30% of American adults are insulin insensitive and 25% have Syndrome X. The Journal of the American Medical Association states that if a patient has three or more of the following symptoms then Syndrome X is present: waist measurement greater than 40” in men (35” in women); triglycerides greater than 150 mg/dl; HDL lower than 40 mg/dl; blood pressure greater than 135/85; or fasting glucose of 110 mg/dl. This means that most people with high cholesterol should reduce sugar and starch consumption and take other steps to bring insulin insensitivity under control.
Problems with sugar and insulin cause weight gain, along with a variety of other health problems. In general, these patients will have a BMI greater than 30. They carry weight around their abdominal area and crave sugar and starch. Getting insulin production under control is the key to weight loss—and there are some products that will help you to do this.
When a patient develops insulin resistance they exhibit the following symptoms:
- Fatigue
- Weight gain and difficult weight loss
- Brain Fog, inability to focus
- Carbohydrate craving
- Periods of hypoglycemia after high carb meals – despite high levels of glucose and insulin.
- Moody and/or depressed
Dietary changes are, of course, necessary. You need to go on a low glycemic diet—avoiding high glycemic foods like refined carbohydrates. Follow a low glycemic diet; avoid refined foods, hydrogenated oils and additives. Eat breakfast—with protein (breakfast should be the largest meal of the day). Eat a lot of fresh produce. Avoiding sugar is often difficult—sugar is addictive. Supplementation should help with cravings (contact our office to. If patients have compliance issues, be patient but be firm in telling them that they need to change their habits. One of the keys is controlling when you eat (see the next paragraph). Eat slowly and eat until you are full. Ideally, only eat three meals per day.
Exercise regularly and stop snacking. The snacking issue is a tough one; many patients are labeled as hypoglycemic. Some feel weak or shaky if meals are delayed or feel the need to snack every two hours (or have been told to do so). You need to wean from this by increasing the time between snacks. When you first eat, you produce insulin which helps to store the calories of the meal. As time goes on, you produce glucagon, which helps to burn the stored calories. The first three hours after eating, insulin is dominant; after three hours glucagon becomes dominant. You cannot lose weight if you keep producing insulin and snacking makes you produce insulin. It is especially important not to eat between dinner and bedtime.
People are so confused about what they should and should not eat. There is so much conflicting information about diet. Registered dieticians talk about the food pyramid, which would give you a diet heavy in grains. Dr. Atkins talks about carbohydrates as being the source of all our health woes. Dr. Dean Ornish and Covert Bailey decry the evils of fat. John Robbins makes a strong case for a totally vegan diet. The Zone diet seeks to give a balance between protein, carbohydrate and fat. Sugar Busters seeks to reduce insulin production. A lot of the information seems to be conflicting and the various dietary gurus have harsh things to say about each other’s diets.
None of the dietary experts can dispute the nutritional rules below. They may offer refinements like, “Watch your fat consumption,” “Watch your carbohydrate consumption” or “Stay away from animal products,” but none of the experts would say there is anything wrong with the following list of dietary advice. There may also be a little controversy about the implications of not following the advice. (Some may dispute that sugar consumption will cause yeast to grow in the intestines, for example, but they would not dispute that consumption of refined sugar is a bad thing.) The advice about water has become controversial, but drinking a lot of water isn’t a problem if you are not drinking a lot of coffee, tea, sodas or other drinks.
- Drink plenty of water each day: You need water to keep your cells hydrated and protected, to eliminate waste and ensure the health of your mucus membranes. Adequate hydration will improve a number of health problems including sinusitis, constipation, inflammation, allergies, fatigue, joint pain, headaches and many other afflictions.
Your body cannot adequately eliminate waste products without enough water. If toxic chemicals or heavy metal poisoning is at the root of your health problems you will have a much easier time getting better when you are properly hydrated. Drink more water and less soda, coffee, tea or juice.
- Eat plenty of vegetables: Plenty means that at least ½ to ¾ of the food you eat (by volume). Vegetables are very high in fiber, vitamin C, folic acid and minerals. They provide you with many health benefits, such as the following:
- Fiber in vegetables slows the absorption of fat and toxins. One of the best ways to lose weight is to eat plenty of fiber. Eating adequate fiber can help normalize cholesterol levels and blood pressure.
- Vegetables nourish normal flora, which in turn nourish the lining of the GI tract, produce vitamins and inhibit yeast and other undesirable organisms.
- Vegetables speed up bowel transit time, which reduces bowel toxicity and prevents irritation of the GI lining.
- Vegetables contain folic acid, which is necessary to produce serotonin (preventing depression and overeating), increases energy and helps reduce the chances for a heart attack.
- The minerals in vegetables help prevent osteoporosis. (Other nutrients besides calcium are important for healthy bone.) Minerals are also important enzyme co-factors, so most major functions of the body are dependent on minerals.
- Eating vegetables can reduce the instance of cancer and heart disease, increase your energy and mental clarity, reduce the problems caused by bowel and liver toxicity, help reduce the symptoms of allergies, asthma, arthritis, skin problems, digestive problems, sinusitis, chronic pain and many other health problems.
- Eating vegetables helps to alkalize the diet. (We will go into the concept of alkaline and acid ash foods in the next section.) Ideally ½ to ¾ of the volume of the food you eat should be vegetables. Corn and potatoes don’t count as vegetables. Fruit is also good for you; it is a good source of vitamin C and fiber. Eating vegetables is stressed here because when people are told to eat more fruits and vegetables, they tend to increase fruit intake but not vegetable intake.
- Avoid deep fried food, trans fats, partially hydrogenated oil and hydrogenated oil: As time passes, we keep finding more bad things about hydrogenated oil and fried foods. Hydrogenation is the food industry’s way of turning liquid oils into solid fats. This gives packaged foods a longer shelf life than if they were made with natural oils. Hydrogenation produces trans fats, which have been linked to a number of health problems such as the following:
- Cancer: Women with higher levels of trans fats in their cells are much more likely to develop breast cancer than women with low levels of trans fats.
- Pain and inflammation become much worse for patients who consume hydrogenated oils. They chemically prevent the formation of natural anti-inflammatory substances that are normally produced by the body. If you suffer from chronic pain or have recently been injured, strictly avoid hydrogenated oil.
- Heart disease: High levels of trans fats create platelet aggregation, which is the beginning of the plaque associated with coronary heart disease. Lately a lot has been written linking inflammation with heart disease.
- Trans fats are incorporated into the cells and make them less resistant to chemicals, bacteria and viruses. This could be a source of immune system problems.
- There may be a link between trans fats and ADD, depression and fatigue. Brain and nerve tissue have a high content of fat. Some researches believe that when trans fats are incorporated into the nerve cells they affect function, creating problems like ADD and depression.
- Muscle fatigue and skin problems are also linked to hydrogenated oils. Most chips and fried snacks contain hydrogenated oils. Hydrogenated oils are found in a lot of packaged foods like crackers, cereals and even bread. They are often found in margarine (margarine is much worse for you than butter); mayonnaise; and a lot of bottled salad dressings. Read labels.
Not all fats are bad for you. Permissible fats include raw nuts (not roasted), virgin or extra virgin olive oil and avocados.
- Avoid refined sugar: The average American eats 150 pounds of refined sugar per year. Compare that to seven pounds per year consumed in England in 1750. Refined sugar increases insulin and adrenal hormone production and can cause the following health problems.
- Increased production of adrenal hormones causes the body to excrete essential minerals.
- Sugar consumption increases the body’s need for vitamins B and C.
- Eating a lot of sugar aggravates many of the problems we associate with emotional stress. Sugar stresses the adrenal glands.
- Sugar feeds yeast and other one-celled organisms found in the bowel, causing them to multiply. These organisms produce toxins, irritate the lining of the GI tract and take the place of normal, more beneficial flora, thus removing the benefits of helpful bacteria.
- Eating sugar causes blood sugar swings. Blood sugar increases immediately after consuming sugar, prompting the body to produce insulin. Excess insulin creates more sugar cravings.
- Eating sugar creates insulin insensitivity. More sugar is eaten, more insulin produced, etc. This stresses the pancreas and sets the stage for adult-onset diabetes.
- There is a connection between sugar consumption and high cholesterol. Patients with Syndrome X (high cholesterol, high LDL, low HDL and high triglycerides) often have the problem because of consumption of sugar and refined carbohydrates.
- Sugar consumption can make pain and inflammation worse.
- Sugar can cause or aggravate allergies, sinusitis, asthma, irritable bowel, Candidiasis, migraine headaches, fatigue, depression and even heart disease.
- Avoid refined carbohydrates: The average American gets 50% of his or her calories from refined carbohydrates. Refined carbohydrates are grains that have had the fiber, vitamin E, B vitamins, bran and germ removed. In other words, the nutrients have been removed and you are left with the starch. They create all of the same health problems created by refined sugar. Go back and read the problems caused by refined sugar and realize that the list is exactly the same for refined starches
Refined carbohydrates fill you up—but not with vitamins and minerals. This stresses your digestive system and your endocrine system. Eating refined carbohydrates uses up precious vitamins and minerals.
Often people eat refined carbohydrates because they are low in fat and mistakenly think that because they are “complex carbohydrates” that they are actually good for you. Refined carbohydrates include white bread, white rice, and pasta that are not labeled whole grain. Read the labels on bread. Brown-colored bread labeled wheat bread isn’t usually whole wheat. If the label says enriched, white flour on it, you’re not getting a whole grain. Use brown rice instead of white rice.
- Avoid chemical additives: Avoid processed foods and chemicals. The average American consumes 10 pounds of chemical additives every year. This has had a devastating effect on our health. The FDA tests single additives, but no one has any idea what combinations of additives do to us. Stay away from packaged foods with chemical additives and you will be much healthier.
- Eat slowly, chew your food thoroughly: Ideally, chew your food until it is liquid. You will be satisfied with less food and you will have better digestion. Your saliva has enzymes that facilitate digestion. Also, it is easier to digest small particles than large ones. Most people eat too fast. Not chewing well stresses your digestive system and can lead to poor absorption of nutrients, digestive problems like gas and bloating and promote the growth of harmful bacteria in the digestive tract.
- Never skip meals: Skipping meals stresses your adrenal glands. If you are trying to lose weight, not eating is a poor strategy because your metabolism will slow down to accommodate the reduction in calories. As a result you become fatigued and will ultimately gain weight.
Because eating this way may be different from your current habits, here are some daily menu suggestions.
| Day 1: | Breakfast | Apple with almond butter |
| Lunch | Tuna (mix it with olive oil chopped onion and celery); celery stalks, carrot sticks or cucumber slices | |
| Dinner | Sweet potato (you can use some clarified butter, which is alkaline), large green salad (oil and cider vinegar) and mixed, cooked vegetables. | |
| Snacks | Any fruit, nuts or any vegetable | |
| Day 2: | Breakfast | Oatmeal |
| Lunch | Turkey, large green salad | |
| Dinner | Brown rice, cooked vegetables, large green salad | |
| Snack | Any fruit, nuts or any vegetable | |
| Day 3: | Breakfast | Quinoa |
| Lunch | Chicken vegetable soup, large green salad | |
| Dinner | Chicken, large green salad, cooked vegetables | |
| Snacks | Any fruit, nuts or any vegetable | |
| Day 4: | Breakfast | Melon |
| Lunch | Hommus, taboule, goat feta cheese and cucumber slices | |
| Dinner | Beef vegetable soup, large green salad | |
| Snack | Any fruit, nuts or any vegetable. | |
| Day 5: | Breakfast | Vegetable omelet (chopped onion, spinach, tomatoes and bell peppers [if nightshades are not a problem for you]). |
| Lunch | Stir fried vegetables and brown rice | |
| Dinner | Broiled salmon, avocado and a green salad |
Try to dominate your diet with raw foods. If your meals have a lot of cooked food, add raw vegetables to your diet. If you must snack, snack on raw vegetables (it is better not to snack, if you can avoid it). Another way to get raw, alkaline food in the diet is to make fresh vegetable juice. If you are busy, simply eating protein with a lot of vegetables is a quick, easy way to make a meal. For example, you can broil a chicken breast, boil some broccoli and make a large salad. It’s fast and it’s fairly alkaline. Another strategy for busy people is to make stews or soups and eat them throughout the week. Just snack on raw vegetables to make sure that you get enough raw food.
In restaurants it isn’t that difficult to eat a relatively alkaline meal. In an Italian restaurant you can order chicken, fish or meat with cooked vegetables and a large salad. Even at McDonalds you can take the bun off of your quarter-pounder and order a salad. McDonalds even has a salad with chicken in it. Many fast-food restaurants now have salad bars. Some will question the quality of even the “good” food at a fast-food restaurant, but the issue here is how to get the best possible meal in a given situation. In a Mexican restaurant you can order fajitas without the tortilla. In a Chinese or Thai restaurant you can get stir-fried vegetables; you can also get a non-fried spring roll as an appetizer.
Raw foods are very good for you. There may be some validity to the argument that we consume the energy from the food we eat. Raw foods have enzymes and higher levels of vitamins like folic acid and vitamin C. Some people, however, have problems when they eat a lot of raw vegetables. If you are such a person, call this to the attention of your health care practitioner. You may need nutritional support for the gall bladder.
Everyone is different and approaches dietary discipline differently. It is strongly suggested that you follow the above dietary rules strictly for at least 30 days. Should you do that, you will get a very good idea of how good a good diet will make you feel. This will make future discipline much easier. Some people may have some difficulty, so we have put together a minimal program. Following it, with the proper supplementation should make it easier to have the discipline to follow all of the necessary dietary changes in the future.
Supplementation Also Helps
If anyone is asked to think of a single nutrient that relates to glucose tolerance, the first thing that comes to mind is chromium. In fact there is a lot of research supporting the idea that chromium is a valuable supplement for people with glucose and insulin issues. People don’t always think of magnesium when it comes to this issue, but there is a fair amount of research supporting magnesium supplementation for insulin insensitivity and poor glucose tolerance.
An observational study appearing in the Journal of the American College of Nutrition (2006; 25(6): 486-92) found that subjects who consumed more magnesium in their diets. The subjects were 1,223 men and 1,485 women without diabetes. Food frequency questionnaires were given to participants of the Framingham Offspring Study and it was found that subjects in the highest quintile of magnesium consumption were better insulin sensitivity than those in the lowest quintile.
In a double-blind, placebo-controlled study appearing in the American Journal of Clinical Nutrition (1992;55:1161-1167), looked at the relationship between glucose tolerance and magnesium status. The subjects were 25 young, healthy men and 12 elderly men. They were given the equivalent of 360 mg. of magnesium or a placebo over a period of four weeks. In the group receiving the magnesium, red cell magnesium levels and the microviscosity of the red cell membranes improved. Magnesium affects insulin secretion and is necessary for the glucose transport system. It is also involved with energy production and an important cofactor for phosphoylation.
It is estimated that 25% of the diabetic population is magnesium deficient. Lethargy, weakness, irritability, confusion, vertigo, paresthesia, anorexia, nausea, vomiting, and tetany are possible symptoms in magnesium deficiency. Diabetic complications include high blood pressure, cardiac arrhythmias, retinopathy, mineral homeostasis, dyslipidemia, and reduced release of insulin—all of which can be the result of insufficient magnesium.
Of course if insulin insensitivity is a problem, other nutrients are of value. Chromium, zinc, B vitamins, selenium, antioxidants and omega-3 fatty acids are all important nutrients for those who are insulin insensitive, diabetic or who have syndrome X.
A pilot study, published in the December 2007 issue of the American Journal of Clinical Nutrition, shows that omega-3 fatty acids may help to reduce fat in type-2 (non-insulin dependent, or adult onset) diabetics. The subjects, 27 women with type-2 diabetes, were given either three grams of fish oil or a placebo for two months.
The women receiving the omega-3 oil had a reduction in total fat and in the size of their fat cells. Also, the supplementation also favorably affected the lipids in the blood, possibly reducing the tendency for arterial plaque formation. Taking omega-3 fatty acids reduced triglycerides and improved the ratio between HDL (“good” cholesterol) to triglycerides. There was also a reduction in the expression of some inflammatory genes found in the fat. This was a small study, but the indications are that omega-3 fatty acids can help diabetics to lose weight and to reduce their risk for heart disease.
A Sample Supplementation Protocol
Of course, supplementation should be tailored to the individual. Call our office for an evaluation and we will help put together a nutritional program designed specifically for you.
- A multivitamin (designed for glycemic control): Many of the companies who sell to chiropractors sell a product that has a lot of chromium, B vitamins, magnesium and other nutrients to help the patient will glycemic control.
- Fish oil: One of the many good things that fish oil does is to help with glycemic control; it also helps to lower cholesterol.
- Phosphatidyl choline Works like a fat detergent; it also helps with adrenal issues. Many of your patients needing to lose weight have high cortisol production. Interesting side note—this is good for exercise-induced asthma (as is fish oil).
- Phosphorus: Insulin insensitivity is an acidic condition; phosphates help to buffer. Phosphorus also helps with bone loss (a lot of osteoporotic women love their carbs). Sugar upsets the balance between calcium and phosphorus.
- Magnesium: Magnesium is also nature’s muscle relaxer, so give it to patients with tight muscles. A woman who is magnesium deficient often will have tender breasts and mood swings related to her cycle. Magnesium causes the stools to soften, so if the patient gets diarrhea, lower the dosage.
Don’t forget to exercise
Research appearing in the March 23, 2003 issue of Diabetes Care [26:557-562] followed 18 sedentary men and women for six months. Participants exercised between three and seven days each week by walking for a half-hour. At the end of the study, researchers examined insulin sensitivity and levels of blood fats, such as cholesterol. None of the subjects lost weight during the study period, but they did enjoy an increase in insulin sensitivity. The researchers concluded that exercise alone increased insulin sensitivity—even without weight loss. The researchers concluded that even moderate exercise, without weight loss or loss of abdominal fat, can improve indicators of glucose and fat metabolism and lower the risk for developing type-2 diabetes.
Please feel free to call our office with any questions.
Lifestyle Changes Better Than Drugs for Diabetes
It is possible to improve insulin insensitivity, metabolic syndrome and even type 2 diabetes with supplementation and lifestyle changes. This is supported by scientific research. There was a recent study that appeared in The New England Journal of Medicine (February 7, 2002;346:393-403). Men and women at high risk of developing type 2 diabetes can reduce this risk by losing weight and exercising, study findings show. The diabetes drug Glucophage can also cut diabetes risk if given preemptively, but not as dramatically.
About 8% of US adults have type 2 diabetes, in which the body loses the ability to respond properly to the blood sugar-regulating hormone insulin. There are well-known risk factors for the disease, including high blood sugar levels after fasting, being overweight, and living a sedentary lifestyle.
To determine whether targeting lifestyle factors with weight loss and exercise, or giving at-risk patients Glucophage, which helps the body respond better to insulin, would cut diabetes risk, the researchers compared these two approaches with an inactive placebo in more than 3,200 nondiabetic men and women.
The average age of study participants was 51, and all had high blood glucose levels. Their average body mass index (BMI) was 34. BMI is a measure of weight in relation to height, and a person with a BMI of 30 or higher is considered obese.
Study participants were randomly assigned to a placebo, 850 milligrams of Glucophage twice daily, or a lifestyle change program intended to help them lose at least 7% of their weight and engage in 150 minutes of physical activity per week.
During the follow-up period, which lasted nearly 3 years, the investigators found that patients in the lifestyle intervention group saw the greatest reduction in their diabetes risk. They had a 58% lower risk of developing type 2 diabetes than people in the placebo group. Those given Glucophage cut their diabetes risk by 31%. The lifestyle program was significantly more effective than Glucophage therapy in all age groups. This study shows that type 2 diabetes is not inevitable. It is not necessary to wait until a person has type 2 diabetes to begin doing something about it.
Glycemic Index and Glycemic Load
Low values for glycemic load and glycemic index are best for people with insulin insensitivity
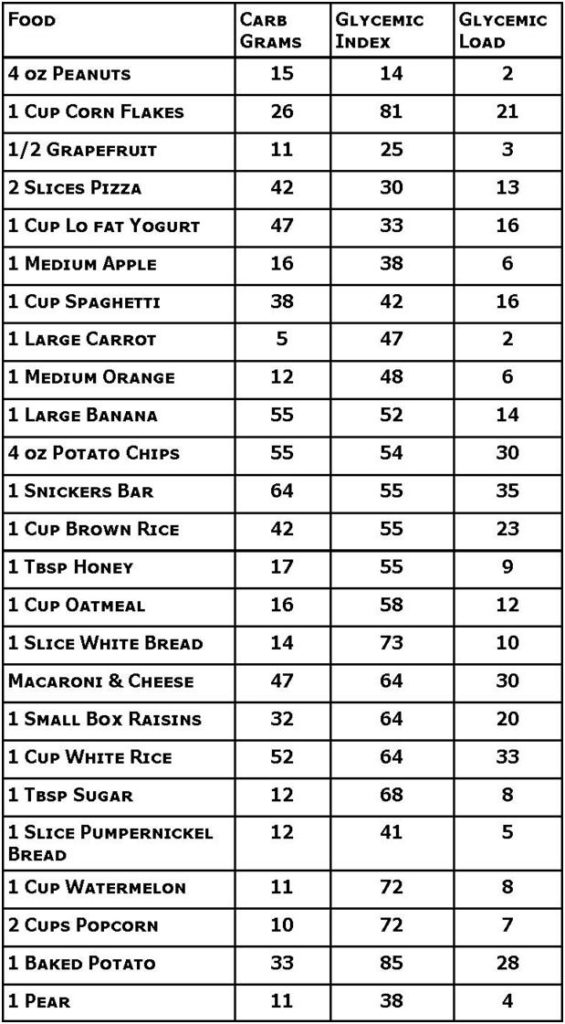
In one study, Supriya Krishnan, of Boston University School of Public Health, and colleagues examined data from 40,078 US women who filled out a food questionnaire in 1995. The glycemic index and glycemic load (a measure of the amount of carbohydrates from glucose) were calculated. The women answered follow-up questions every two years about their weight, health and other factors. During eight years of follow-up, 1,938 participants developed type 2 diabetes. Women who ate high-glycemic index foods or a diet with a high glycemic load had a higher risk for diabetes. However, women who ate more fiber from grains had a reduced risk.
Krishnan’s results showed that those women with a body mass index (BMI) of less than 25, who ate about 1.5 grams of fiber per day were 59 percent less likely to develop diabetes than women who ate about 8.3 grams per day.
Because high-glycemic index foods increase blood glucose levels significantly, they increase the body’s demand for insulin. This can contribute to problems with the pancreas, which produces insulin, and may eventually lead to diabetes, the researchers said.
Krishnan said: “Our results indicate that women can reduce their risk of diabetes by eating a diet that is high in cereal fiber. Incorporating fiber sources into the diet is relatively easy: a simple change from white bread to whole wheat bread or substituting a cup of raisin bran or oatmeal for a cup of corn chex or rice chex will move a person from a low fiber intake category to a moderate intake category, with a corresponding 10 percent reduction in risk.”
A second study led by Raquel Villegas of Vanderbilt University Medical Center followed a group of 64,227 Chinese women for an average of five years. During the study, 1,608 of the women developed diabetes. Women who consumed more carbohydrates overall were more likely to develop diabetes, they found.
The team noted that women who ate diets with a higher glycemic index and who ate more staples such as bread, noodles and rice specifically also had an increased risk. Women who ate 300 grams or more of rice per day were 78 percent more likely to develop diabetes than those who ate less than 200 grams per day.
Villegas noted that: “Given that a large part of the world’s population consumes rice and carbohydrates as the mainstay of their diets, these prospective data linking intake of refined carbohydrates to increased risk of type-2 diabetes mellitus may have substantial implications for public health.”






